Overview
Coeliac disease is an autoimmune condition where individuals can have an adverse response to gluten when they eat it. Gluten is a protein found in wheat, barley and rye. It is typically a healthy and safe food to eat. However, for those living with coeliac disease, when gluten is eaten it causes damage to the lining of the small bowel because the body ends up attacking its own cells. This can impair nutrient absorption from food, contribute to symptoms and cause long-term health problems. Coeliac disease is not an allergy or intolerance. The only treatment that exists for coeliac disease is a lifelong gluten-free diet.
Studies show that approximately 1 in 100 people in the UK have coeliac disease. Some people who have coeliac disease don’t actually know they have it and may only experience mild symptoms and others may experience no symptoms at all. Coeliac disease is sometimes diagnosed while looking into another health problem. It is thought that nearly 7 out of 10 people remain undiagnosed. This means there are about half a million people living with coeliac disease unknowingly.
Causes
The exact cause of coeliac disease is not fully understood as it involves a complex interaction between genes and environmental factors. More females assigned at birth tend to be diagnosed than those designated male at birth. The average age of diagnosis is between 40 and 60 years old, but people can be diagnosed at any age once gluten is introduced in the diet.

Genetics play an important role in the development of coeliac disease. Therefore, being a first-degree relative of someone with coeliac disease increases the risk of developing the condition. To develop coeliac disease, a person must have a mutation on the HLA-DQ gene. These mutations are common- about 4 in 10 of the general population carry them. However, not everyone with the mutation will develop coeliac disease. Many different environmental factors can trigger the development of the condition in genetically predisposed individuals. Conditions like Downs or Turner syndrome, type 1 diabetes or thyroid problems can increase the likelihood of developing coeliac disease. The relationship between these conditions and coeliac disease development is unclear, but it is apparent that having coeliac disease increases the risk of developing other autoimmune conditions. Research to learn more about coeliac disease and find out the exact causes of it is ongoing.
What does coeliac disease look like?
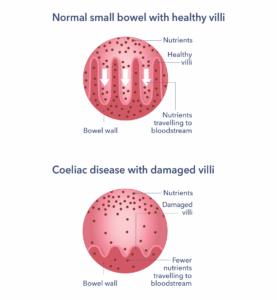
The villi in the small intestine are in charge of nutrient absorption. In a person with coeliac disease, when gluten is eaten, the villi become damaged and inflamed. They will look shorter and stubbier. This means that fewer nutrients can pass into the bloodstream and that the small intestine is damaged.
How can coeliac disease affect the body?
In some people with coeliac disease, gluten-induced damage leads to the villi being almost completely flat. This is called villous atrophy. This reduces the bowel’s surface area, meaning there is a reduced absorption of nutrients. This can lead to nutrient deficiencies in the body. Avoiding gluten allows the villi to recover over time. However, coeliac disease remains a lifelong condition and requires a lifelong gluten-free diet to keep it treated.
The main ways that coeliac disease can affect the body is:
- Physical discomfort: bloating, abdominal discomfort, unexplained weight loss, a change in bowel habit to diarrhoea or constipation.
- Shortage of essential nutrients: this can lead to deficiencies and other conditions. Examples are osteoporosis (causing bone fractures) or anaemia (causing symptoms of lethargy). Many people can experience extreme fatigue.
- Symptoms beyond the gut: occasionally there can be problems with the nerves to the extremities causing numbness and tingling to the hands and feet. Some people may also experience other non-digestive symptoms like brain fog, balance problems, mouth ulcers and infertility, amongst other symptoms.
- Dermatitis herpetiformis: this is a skin disease that is associated with coeliac disease and that consists of skin rashes that can also blister. It is common to see around the elbows, knees, shoulders and face. If this is present, you can get referred to a dermatologist and have a skin biopsy to diagnose it.
Diagnosis
Coeliac disease has similar symptoms to other conditions like Irritable Bowel Syndrome, leading to possible misdiagnosis if it is not tested properly. An accurate diagnosis is vital. If you suspect you have coeliac disease, go to your GP. The doctor will carry out an examination and take a medical history. If coeliac disease is suspected, the following tests may be performed:
Blood tests
Two antibody tests are carried out and must be done whilst gluten is still being eaten for at least 6 weeks before each blood test.
- Tissue Transglutaminase (TTg) (first choice test)
- Endomysial antibody (EMA) (if TTg is weakly positive)
The results of these tests alone may be enough to diagnose coeliac disease for some people depending on the blood values, the symptoms and the age of the person being investigated. However, in most situations an additional test in the form of an endoscopy is also required to confirm the diagnosis with certainty.
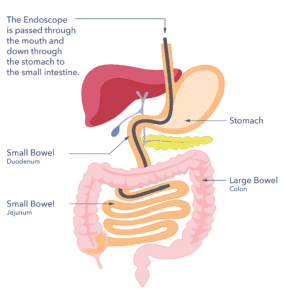
Endoscopy
This involves inserting a thin, flexible tube through the mouth and down into the small intestine. Following that, biopsies are taken. This can be uncomfortable, but it should not be painful. Any abnormalities that indicate coeliac disease will be shown on the biopsy samples once they are processed. This confirms the diagnosis with certainty.
It is important to continue eating gluten for six weeks before the blood tests or endoscopy tests are done to ensure accurate results. An abnormal reaction won’t be found if you’re not eating enough gluten. Discuss things with your GP if this is a problem. The treatment of coeliac disease requires a gluten-free diet for life so it’s crucial to be confident that the diagnosis is right.
Symptoms
Coeliac disease symptoms can vary between people. In children, symptoms can include diarrhoea, vomiting or a failure to gain weight. Adults often experience a combination of symptoms. A typical symptom is diarrhoea with bloating or discomfort in the abdomen.
People don’t always have symptoms that appear to be related to their gut. Coeliac disease can manifest in a variety of ways. It is important that people with associated conditions like Autoimmune Thyroid Disease and Type 1 Diabetes be tested. Some other symptoms may include:
- Persistent lethargy (tired all the time).
- Loss of sensation of fingers and toes.
- Headaches and migraines.
- Skin rashes (called dermatitis herpetiformis).
- Whilst diarrhoea is common, constipation can also occur.
- Unexplained weight loss.
- Feeling generally unwell.
- Persistent mouth ulcers.
- Unexplained infertility or repeated miscarriage.
- Lack of absorption of vitamins and minerals like iron, B12 and folate.
How will coeliac disease affect me over time?
Coeliac disease is a lifelong condition. Sticking to a gluten-free diet is the only treatment that restores the gut and keeps it healthy long-term. If the gluten-free diet is not followed there can be reduced nutrient absorption which may lead to issues such as anaemia (low iron levels) or osteoporosis (weakened bones). There is also a slightly increased risk of certain cancers in individuals who continue to consume gluten. However, this risk is a lot smaller if gluten is avoided for life. Coeliac disease may also cause infertility in women designated female at birth if they remain undiagnosed. This is usually resolved with a gluten-free diet. It is worth noting that the small bowel can take from 2 to 5 years to fully recover, depending on the amount of initial damage present.
The gut is linked to the brain, and so coeliac disease can cause neurological symptoms like headaches and ‘brain fog’. Nearly 4 in 10 adults will have neurological symptoms when diagnosed with coeliac disease. These often improve with a gluten-free diet. If they do not, you may need a referral to a neurology specialist. If you have coeliac disease and exclude gluten from the diet, life expectancy shouldn’t be affected.
Treatment
The treatment for coeliac disease is to follow a lifelong gluten-free diet. If you are diagnosed with coeliac disease, your doctor will refer you to see a dietitian. They can provide you with information on how to avoid gluten. It is important to know how to maintain a balanced gluten-free diet.
What is gluten?
Gluten is a protein found in wheat, barley and rye and products made using these grains. You may find it useful to remember the acronym BROW which stands for the main grains that should be identified and avoided. These are barley, rye, oats and wheat. However, it is important to bear in mind that most people living with coeliac disease can eat oats if they are gluten-free and we will explain who may not be able to eat them below.
What foods contain gluten?
Breads, pastas, breakfast cereals, cakes, biscuits generally contain gluten. Many other packaged foods can also contain gluten. For example, flour is used as a thickener in many cooking sauces and barley is used in making most beers and lagers. Foods can also get contaminated with small amounts of gluten during production or processing if gluten comes into contact with gluten-free food. This is why it is important to always avoid gluten in ingredients and from a cross-contact point of view. We know that very small amounts of gluten can cause problems for people with coeliac disease.
Choose only gluten-free varieties of oats, as they can be at risk of gluten cross- contact during processing. These are a great source of soluble fibre. Check the labels to ensure they are gluten-free. A small number of people react to avenin, a protein found in oats that is like gluten (even ‘gluten- free’ versions). If you continue to have symptoms despite following a gluten-free diet, this may be why and its worth discussing this with your dietitian or doctor.
Grain suitability
Some flours made from naturally gluten-free grains may have cross-contact risks, so always read the label. Flours labelled gluten-free will be free from gluten cross-contact.
Food labelling
Food manufacturers are required to label allergens, including gluten, on ingredients lists in bold. Check labels for Barley, Rye, Oats and Wheat (BROW).
Some products without these grains have advisory labelling such as ‘May contain gluten’ or ‘Made in a factory handling wheat’. This shows a risk of cross-contact with gluten. If you are unsure of a product’s suitability, it’s usually best to avoid it. Coeliac UK charity can help with clarifying the suitability of specific products.
Be cautious when travelling abroad as food labelling rules may not be as strict in countries outside the UK. Most European countries have similar regulations in place. Travelling further can be safe with research and planning.
What foods are suitable for a gluten-free diet?
Many foods are suitable for people living with coeliac disease. Learn to check foods and find gluten-free sections of shops. Naturally gluten-free foods can be found throughout shops too. These often prove to be cheaper options. The Crossed Grain symbol (see below) is also an easy way of identifying foods you can eat and ensures there is an additional layer of testing to guarantee safety.
Labelled gluten-free foods
These foods can be consumed by people with coeliac disease. They meet a specific legal standard of being tested to have no more than 20 parts per million gluten (sometimes written as ‘<20 ppm’). This will be labelled on the packaging of food products.
Manufacturers and supermarkets make a wide variety of gluten-free foods. Try a variety of these to see which you most enjoy.
In Wales and Northern Ireland, a range of gluten-free foods are available on prescription from your doctor. Some places in Wales use a top-up card scheme to get these products. In Scotland gluten-free foods are available on prescription through your pharmacist. These ranges may include bread, flour mixes, pasta, crackers and breakfast cereals.
Integrated Care Boards (ICBs) manage GP surgeries in England. These organisations decide their own prescribing policy. These vary according to where you live. The ICBs can restrict or suspend the availability of gluten-free products on prescription in some areas. You can check with your pharmacist to find out if prescription gluten-free products are available in your area.
Foods made without gluten containing ingredients
Many foods are prepared without gluten containing ingredients. There are measures in place to minimise the risk of cross contact. These foods can be identified by reading labels. If you are unsure, look at Coeliac UK’s resources ‘The Eat Well, Live Well’ food and drink directory. There is also a Coeliac UK digital application that can help to identify these products.
Eating out
Restaurants are increasingly trying to help by labelling gluten- containing dishes. Caterers are required by law to be able to provide information about gluten in all their dishes. If the information is not easily seen it must be clear where it can be found. Coeliac UK has an accreditation scheme for restaurants and a symbol that can be used on a menu. The symbol tells you that the dish is gluten-free according to the law. This covers all aspects of gluten-free preparation and ensures training is in place to reduce the risk of gluten cross-contact. It is still important to inform staff of your requirements.
Initially, eating outside the home can appear daunting. It is important to not let a gluten-free diet become socially restrictive. Over time, you will learn how to navigate social situations and ask the right questions about how your meal is prepared. If you have any concerns, please discuss this with your dietitian.

Support
Does my coeliac disease need monitoring?
As you might develop problems in the future, it is important to monitor your health long-term. It is recommended that you have an annual check-up, including blood tests to check for anaemia or nutrient deficiencies. If your symptoms persist or new ones arise, ask for another referral to the gastroenterologist and dietitian if you not already under their care.
Your doctor may arrange for you to have a bone scan (a DEXA scan) at one of your follow-up appointments. This will look for any sign of bone thinning so it can be treated early, since some people can have weaker bones due to not absorbing enough calcium and vitamin D. Some people with coeliac disease may also have impaired spleen function. This is an important organ for our immune function, so vaccinations against flu and pneumonia infections may also be advised.
What to ask your doctor
- Where are the best sources of information about living gluten-free?
- Can you refer me to a dietitian?
- Are there any support groups for coeliac disease in my area?
- Should my close family be tested for coeliac disease?
- Are gluten-free prescriptions available in my area?
- How often will you be monitoring me for to ensure coeliac disease is well controlled?
- Should I have a bone scan?
What other resources and organisations can help?
Coeliac UK is the leading UK charity supporting people diagnosed with coeliac disease.Their membership services include:
- Helpline supported by expert dietitians and advisers.
- Access to the latest gluten free products and food and drink information. The printed version updated monthly, use online version for most up to date information.
- Recipe information, inspiration and advice on gluten free cooking and baking.
- Over 50 travel guides with information on where to eat out and shop, alongside useful translations.
- Venue guides on over 3,000 accredited venues as well as others’ recommendations on where to eat out.
- Award winning digital applications: Gluten Free Food Checker (which can scan barcodes and to identify suitable foods and Gluten Free On The Move (which can help identifying suitable venue when you’re away from home)
- Local groups and peer support through Member2Member scheme.
- Live Well Gluten Free magazine.
- Useful educational videos and dietetic workshops.
A Priority Setting Partnership (PSP) has been completed which identifies the top ten research priorities for coeliac disease. You can find out what these are from Coeliac UK.
Discover more:
Copyright © 2026 Guts UK. This leaflet was published by Guts UK in 2023 and will be reviewed in 2025. The leaflet was written by Guts UK and reviewed by experts in coeliac disease and has been subject to both lay and professional review. All content in this leaflet is for information only. The information in this leaflet is not a substitute for professional medical care by a qualified doctor or other healthcare professional. We currently use AI translation tools on our website, which may not always provide perfect translations. Please check for further explanation with your doctor if the information is unclear. ALWAYS check with your doctor if you have any concerns about your health, medical condition or treatment. The publishers are not responsible or liable, directly or indirectly, for any form of damages whatsoever resulting from the use (or misuse) of information contained or implied in this leaflet. Please contact Guts UK if you believe any information in this leaflet is in error.